The paper is accepted in JIAS.
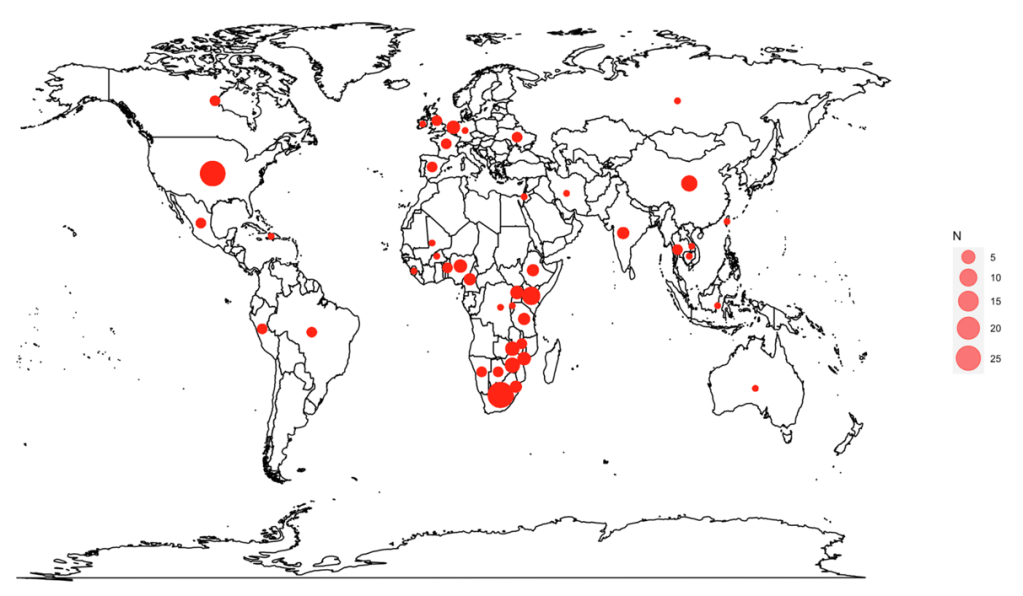
Figure 1. Geographic location of cost-effectiveness modeling of PrEP intervention and implementation strategies (Number of studies (N)=128). Note: Six studies were conducted in the Sub-Saharan African region, but did not specify the countries assessed, so they are not shown on the map.
Summary
Why did we conduct this study?
HIV pre-exposure prophylaxis (PrEP) is a medicine that helps protect people from getting HIV. Over the years, new types of PrEP have been developed–from the first daily oral pill to newer options like long-acting injections. Different ways of delivering HIV PrEP (e.g., phone apps, community organizations, mail order, clinic) have also been developed to tailor to people’s needs.
There is a lot of evidence that HIV PrEP works extremely well, but it takes resources (e.g., medication costs, health care delivery costs) to roll out PrEP. This is where evaluations of costs and benefits come in. Policymakers, health leaders, and community-based organizations need clear and up-to-date information about the costs and benefits of different types of HIV PrEP and different ways of delivering it. This information helps decision-makers consider how to fund and deliver HIV PrEP so that the people who may be at risk of acquiring HIV can access and benefit from HIV PrEP.
We reviewed all the available research on evaluating the costs and benefits of HIV PrEP to map out how research on this topic has changed over time. Our goal was to find out what information is still missing to help guide HIV prevention efforts and support decision-making.
What did we do?
We searched five major research databases for studies that evaluated the costs and benefits of HIV PrEP, up to August 21, 2025. We included studies from all countries and in all languages.
We looked at how research on the costs and benefits of HIV PrEP has changed over time. This included looking at who received HIV PrEP in the studies, which groups of people or regions were represented in existing studies, the types of HIV PrEP studied (e.g., daily oral pills, long-acting injections), and how HIV PrEP was delivered. We also examined whether studies only considered healthcare costs or included broader societal impacts such as peoples’ out-of-pocket expenses and time missed from work in addition to healthcare costs. Lastly, we examined how studies compared HIV PrEP with other HIV prevention methods, including whether these other HIV prevention programs may grow or change over time.
What did we find?
We found 128 studies that looked at the costs and benefits of HIV PrEP. Most studies focused on countries across Sub-Saharan Africa and North America, and on gay, bisexual, and other men who have sex with men. Fewer studies looked at other regions (e.g., Latin America and the Caribbean) and/or other groups at high risk of getting HIV, including sex workers and their clients, people involved in mixed HIV status relationships (e.g., one partner living with HIV and one partner not living with HIV), adolescent girls and young women, and injection drug users.
Most studies focused on early forms of HIV PrEP, such as daily oral pills, with fewer evaluating newer forms such as long-acting injections. Few studies considered broader societal costs and impacts of HIV PrEP, compared different forms of HIV PrEP to each other, or reflected how existing HIV prevention programs may change over time in their analyses.
What do these findings mean for public health?
Existing research on the costs and benefits of HIV PrEP does not (yet) fully reflect the current HIV epidemic and the different HIV prevention programs currently available. Because of this, policymakers and health leaders may find it difficult to decide which types of HIV PrEP and delivery methods should be funded or expanded.
We recommend that future research should compare the costs and benefits of different forms of HIV PrEP to each other, consider social and economic impacts beyond healthcare costs, and compare HIV PrEP to current HIV prevention programs, including potential changes and expansion of these programs over time. This information will help ensure shrinking budgets are used wisely and are nimble enough to ensure HIV PrEP and other HIV prevention programs can reach the people who need them most and help prevent HIV transmission in an evolving landscape of HIV epidemics and HIV programs.
This work was led by team member Min Xi, and in partnership with our close collaborator and health economist Dr. Kednapa Thavorn at the Ottawa Hospital Research Institute.
Funding
This study was funded by an Early Researcher Award (ER17-13-043), a Canadian Institutes for Health Research Foundations award (FDN-143266), and a Canadian Institutes for Health Research Project grant (416186).