The paper is published in the PLOS Global Public Health.
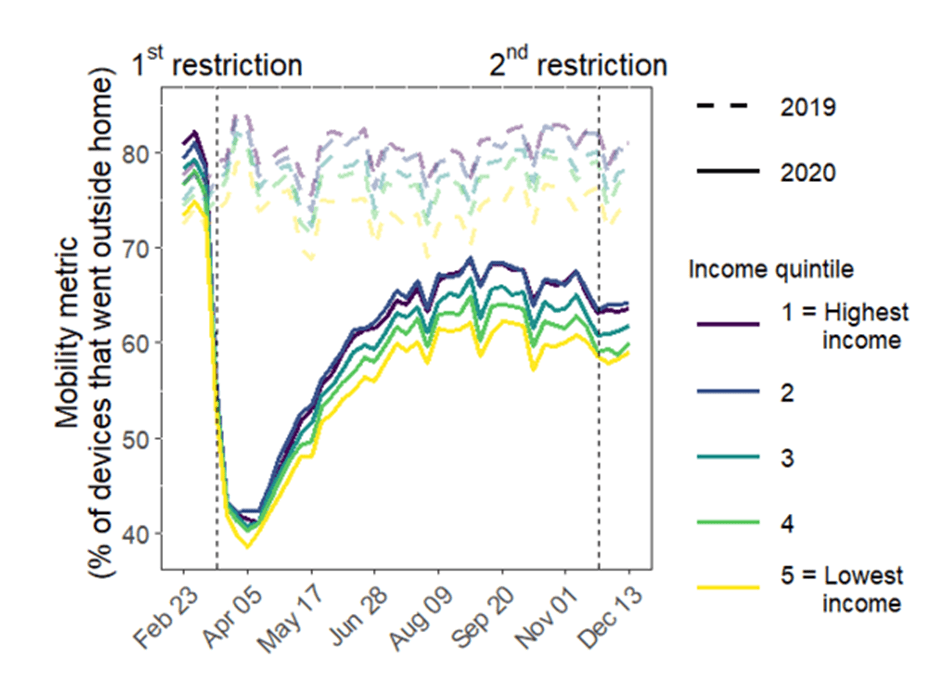
Figure 1. Mobility change stratified by neighborhood-level income quintiles in the Greater Toronto Area, Canada (February 23, 2020 to December 13, 2020). The figure depicts the weekly crude mobility metric by neighborhood-level income quintile. The horizontal dashed lines represent 2019 mobility as pre-pandemic mobility reference, while the solid lines represent 2020 mobility data. The vertical dashed lines depict the two COVID-19 restriction policies under examination: the first restriction enacted on March 17, 2020, across all five public health units (Toronto, Peel, Halton, York, and Durham) in the Greater Toronto Area; and the second restriction enacted November 23, 2020 in Toronto and Peel public health units within the Greater Toronto Area. Income reflects the per-person equivalent income in the household. The neighborhood level is defined at the level of the census tract. Quintiles are weighted by neighborhood-level population.
Why did we conduct this study?
In Canada, as in many other countries, essential workers and lower-income households were disproportionately at risk of SARS-CoV-2 infection. Early in the pandemic, stay-at-home restriction policies were implemented to help limit the spread of the virus outside the home, and in turn, to reduce the “importation of virus” into households. A few studies found these restrictions were associated with smaller reductions in mobility in lower-income neighborhoods. However, these prior studies were not able to account for expected differences in baseline mobility across socioeconomic factors, nor were they able to compare mobility with regions without the restriction policies.
What did we do?
We combined cell phone mobility data with neighborhood-level measures of household income and the proportion of essential workers. We quantified changes in mobility in response to two restriction policies across five regions in Ontario, Canada. We further examined whether reductions in mobility varied by neighborhood-level socioeconomic measures.
The first restriction policy started on March 17, 2020, and was implemented in all five regions. To examine the first policy, we conducted a descriptive analysis of mobility changes by socioeconomic factors.
The second restriction policy started on November 23, 2020, and was implemented in two of the five regions. This means there were two regions with a restriction policy and three regions without restriction policies. Thus, the comparison regions provided a natural experiment with which to conduct a type of analysis that could account for expected versus observed mobility changes (called a difference-in-differences analysis). To examine the second policy, we: a) compared the expected versus observed changes in mobility following policy implementation and b) how socioeconomic factors may or may not modify the relationship between restriction policy and subsequent mobility changes (called effect modification).
What did we find?
We found that:
- The first COVID-19 restriction policy led to large (30-40%) reductions in crude mobility. Reduction in mobility following the first restriction policy was largest in the highest-income neighborhoods and in neighborhoods with the fewest essential workers.
- In contrast, a very small (<1%) reduction in mobility was associated with the second restriction policy. However, there was still evidence of effect modification by income and proportion of essential workers (less pronounced mobility reductions in lower-income neighborhoods and in neighborhoods with more essential workers).
What do these findings mean for public health?
The findings suggest that the effect of restrictions on mobility changes saturate over subsequent restrictions. There is also a saturating effect by socioeconomic factors: with less mobility change is possible in neighborhoods with lower income and in neighborhoods with a higher proportion of essential workers. This means that restriction policies leave a prevention gap by socioeconomic factors. The study highlights the need for additional approaches to reduce health inequities at the intersections of income and occupation when addressing large epidemics of novel and resurging respiratory pathogens.
This research was led by Siyi Wang and co-authored by Linwei Wang, Stefan D Baral, Gary Moloney, Jaimie Johns, Carmen Huber, Jaydeep Mistry, Kamran Khan, Amrita Rao, Naveed Janjua, Tyler Williamson, Alan Katz, Huiting Ma, Mathieu Maheu-Giroux, and Rafal Kustra. It is corresponded by Sharmistha Mishra. The research was supported by funding from the Canadian Institutes of Health Research (grant no. VR5-172683), the Natural Sciences and Engineering Council of Canada Discovery grant, and the Natural Sciences and Engineering Research Council of Canada CANMOD grant (Canadian Network for Modelling Infectious Disease, grant no. RGPID-560516-2020).
elegant! Scientists Create First Synthetic Human Embryo 2025 enjoyable
LikeLike