Why did we conduct this study?
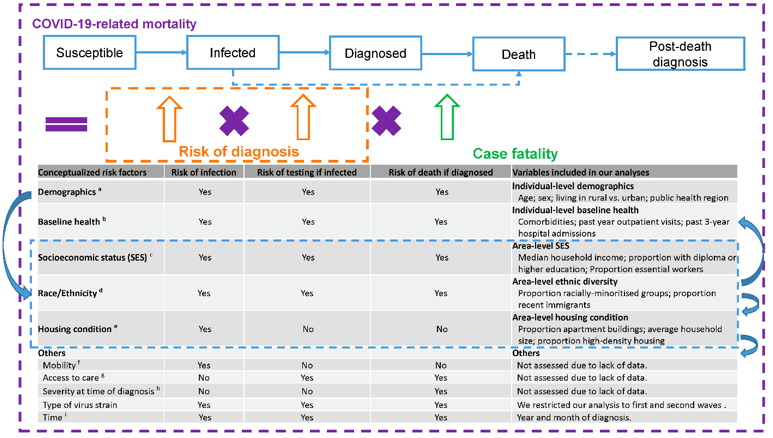
Figure 1. Conceptualization of risk factors for COVID-19–related mortality. Based on the conceptualized factors, we sourced data, where available, at the individual level, otherwise at the area level.
Social determinants of health (SDOH) such as income, education, and race/ethnicity (as proxies for systemic racism) play an important role in COVID-19 outcomes. SDOH can lead to COVID-19-related death via a combination of the following pathways: likelihood of infection, likelihood of diagnosis once infected, and likelihood of COVID-19-related death once diagnosed. Understanding the mechanisms under which SDOH influence COVID-19-related death can help inform pandemic responses to address prevention gaps associated with SDOH.
What did we do?
Using data of 11.8 million adults residing in Ontario, we examined the patterns in COVID-19-related mortality by a set of area-level SDOH factors, including socioeconomic status (median household income, the proportion with a diploma or higher educational attainment, proportion of essential workers), ethnic diversity (proportion racially-minoritized groups, proportion recent immigrations) and housing conditions (proportion apartment buildings, proportion high-density housing, average household size). We assessed whether the mortality patterns by SDOH could be explained by individual-level demographic and clinical factors. We also compared patterns by area-level SDOH in COVID-19-related mortality versus those in non-COVID-19 mortality to understand whether the same patterns of inequities drive both COVID-19 and non-COVID-19-related death. Finally, we examined the patterns by area-level SDOH in COVID-19 case fatality, capturing the influence of SDOH post-diagnosis.
What did we find?
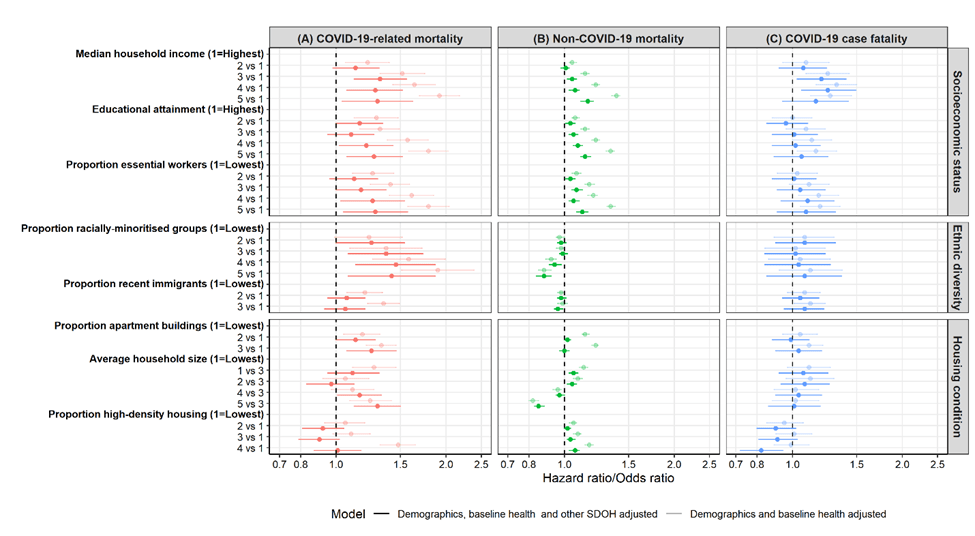
Figure 2. Comparing area-level social determinants of health (SDOH) in COVID-19-related mortality, non-COVID-19 mortality, and COVID-19 case fatality among community dwelling adult populations aged 20 years and older in Ontario, Canada, March 1 2020 – Mar 2, 2021.
Of 11,810,255 individuals, we observed 3,880(0.03%) COVID-19-related deaths and 88,107(0.75%) non-COVID-19 deaths. We found that areas characterized by lower socioeconomic status (including lower median household income, a lower proportion with a diploma or higher educational attainment, and a higher proportion of essential workers), a higher proportion of racially minoritized groups, more apartment buildings, and large vs. medium household size experienced higher COVID-19-related mortality; even after accounting for individual’s demographics, clinical factors, and other area-level SDOH. We also found that COVID-19 has reversed patterns of lower non-COVID-19 mortality among racially minoritized groups, such that areas with a higher proportion of racially minoritized groups experienced higher COVID-19-related mortality. Of all area-level SDOH examined in our study, lower median household income was associated with a higher likelihood of COVID-19-related death after diagnosis.
What do these findings mean for our healthcare systems?
Findings highlight that the role of social and structural inequalities in COVID-19-related mortality primarily stem from proximal exposures leading to SARS-CoV-2 infections; and reach of, and access to, prevention interventions. That is, it is primarily through the ways in which social and structural determinants shape infection risks that led to social and structural inequalities in COVID-19-related mortality. However, the relationship between income and COVID-19-related death post-diagnosis may also reflect delayed diagnosis or access to and quality of clinical care for persons living in lower-income areas.
The goal of pandemic responses should include improving overall population health by addressing disproportionate acquisition and transmission risks and inequitable coverage of prevention interventions associated with SDOH. Tailored strategies include but are not limited to: paid sick leave and improved workplace health and safety protocols and outbreak management; and community-led and community-tailored outreach for testing, effective isolation, and vaccination programs.